Malaria is an acute infectious disease caused by Plasmodium parasites (most commonly P. falciparum and P. vivax) transmitted through the bite of an infected Anopheles mosquito. Once inside the bloodstream, parasites invade red blood cells, multiply, and cause periodic fevers and systemic illness. If left untreated—particularly P. falciparum—malaria can progress to severe anemia, cerebral complications, organ failure, and death.
-
Fever & Chills: Classic “paroxysm” of rising temperature, rigors, then sweating
-
Headache & Muscle Aches: Persistent, often severe headache; generalized myalgia
-
Fatigue & Weakness: Profound lethargy and malaise
-
Gastrointestinal Distress: Nausea, vomiting, abdominal pain, diarrhea
-
Anemia & Jaundice: Pallor from hemolysis; yellowing of skin/eyes in severe cases
-
Splenomegaly: Tender enlargement of the spleen due to parasite clearance
-
-
Mosquito Transmission: Female Anopheles mosquitoes inject sporozoites into the bloodstream during a blood meal.
-
Parasitic Life Cycle: Sporozoites travel to the liver, mature into merozoites, then enter red blood cells where they replicate.
-
Blood Transfusion or Shared Needles (rare): Direct introduction of infected blood can transmit parasites.
-
Congenital Transmission: Rare passage from mother to fetus during pregnancy.
-
-
Travel to Endemic Regions: Tropical/subtropical areas of Africa, South Asia, and South America.
-
Lapses in Prophylaxis: Missing antimalarial prevention doses before, during, or after travel.
-
Immune Suppression: HIV, malnutrition, or chemotherapy reducing natural resistance.
-
Seasonal Rainfall & Standing Water: Increased mosquito breeding following monsoon or flooding.
-
Inadequate Vector Control: Lack of insecticide-treated nets or indoor spraying.
-
-
Rapid Diagnostic Tests (RDTs): Detect histidine-rich protein or lactate dehydrogenase antigens specific to Plasmodium spp., providing results in 15–20 minutes.
-
Microscopic Examination: Thick and thin blood smears stained with Giemsa to identify Plasmodium species, quantify parasitemia, and determine stage (ring, trophozoite, schizont).
-
PCR (Polymerase Chain Reaction): Highly sensitive molecular assay for species confirmation, especially in low-parasite-count or mixed infections; used in reference laboratories.
-
Clinical Evaluation: History of travel to endemic area plus classic fever pattern warrants empiric antimalarial therapy if testing unavailable, especially in high-risk P. falciparum regions.
-
-
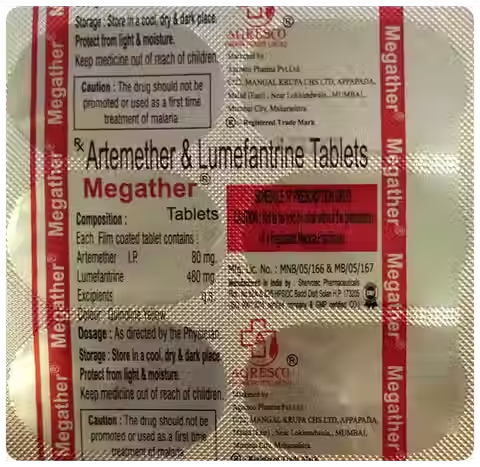
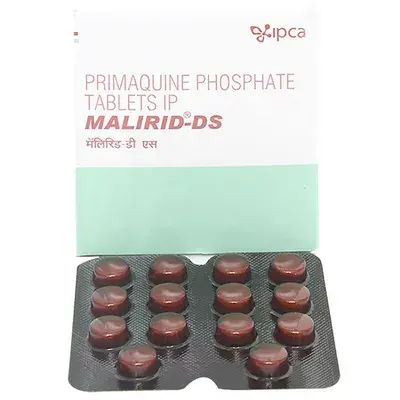
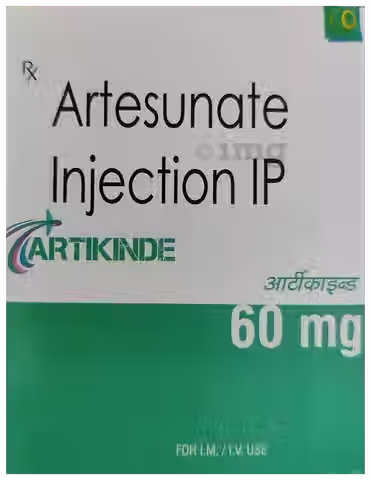
First‐line therapy for uncomplicated P. falciparum malaria is a combined artemisinin-based regimen (e.g., Artemether 40 mg + Lumefantrine 240 mg, twice daily for three days). Chloroquine remains effective in regions where P. vivax or P. ovale are chloroquine-sensitive: 600 mg base once, followed by 300 mg base at 6, 24, and 48 hours. Primaquine (15 mg daily for 14 days) is added to eradicate dormant P. vivax/ovale hypnozoites and prevent relapse; G6PD screening is mandatory before primaquine. Severe malaria requires intravenous Artesunate 2.4 mg/kg at 0, 12, and 24 hours, then daily until oral therapy is possible. Mefloquine (250 mg base weekly) or Doxycycline (100 mg daily) may be used for prophylaxis in endemic travel, started one week before departure and continued for four weeks after return.
-
Q1: How soon after returning from an endemic area should I be checked for malaria?
A: P. falciparum typically causes symptoms within 7–14 days; P. vivax/ovale relapse can occur up to 6 months later. If you develop fever or flu-like symptoms at any time post-travel, seek a malaria test immediately.
Q2: Is resistance to antimalarial drugs a concern?
A: Yes—chloroquine-resistant P. falciparum is widespread in Africa and South Asia. Artemisinin partial resistance has emerged in the Greater Mekong region; combination therapy mitigates this risk.
Q3: Can pregnant women take antimalarials?
A: In the first trimester, use Chloroquine in chloroquine-sensitive regions; Artemisinin-based combos are generally avoided until the second and third trimesters unless benefits outweigh risks. Primaquine is contraindicated in pregnancy.
Q4: Do antimalarial drugs prevent infection completely?
A: Prophylactic regimens (e.g., Mefloquine, Doxycycline, Atovaquone-Proguanil) substantially reduce risk but do not guarantee 100% protection. Preventive measures—mosquito nets and repellents—remain essential.
Q5: What side effects should I watch for when taking Artemisinin-based therapies?
A: Common mild effects include headache, dizziness, nausea, and transient elevation of liver enzymes. Rare neurotoxicity has not been observed at standard doses.