The gastrointestinal (GI) system comprises the esophagus, stomach, small and large intestines, and accessory organs (liver, pancreas). It breaks down food, absorbs nutrients and water, and eliminates waste. When any segment malfunctions—due to excess acid, motility issues, or inflammation—you may experience discomfort and disrupted digestion.
-
Upper GI:
-
Heartburn, acid regurgitation, epigastric pain
-
Nausea, vomiting, bloating, early satiety
-
-
Lower GI:
-
Constipation or difficulty passing stool
-
Diarrhea, loose stools, urgency
-
Abdominal cramps, gas, bloating
-
-
-
Excess Acid Production: GERD, peptic ulcer disease
-
Motility Disorders: Gastroparesis, IBS (irritable bowel syndrome)
-
Infections: Viral or bacterial gastroenteritis
-
Inflammation: IBD (ulcerative colitis, Crohn’s disease)
-
Dietary Factors: Spicy/fatty foods, lactose intolerance, low-fiber diet
-
Medications: NSAIDs causing ulcers, antibiotics triggering diarrhea
-
-
Dietary Triggers: Coffee, alcohol, carbonated drinks, trigger foods in IBS (e.g., FODMAPs)
-
Stress & Anxiety: Alters gut motility and sensitivity
-
Irregular Meals: Skipping meals or overeating
-
Medication Use: Long-term NSAIDs or certain antibiotics
-
Infections & Travel: Exposure to contaminated food or water
-
-
Medical History & Physical Exam: Symptom pattern, weight change, abdominal tenderness
-
Endoscopy/Colonoscopy: Direct visualization of esophagus, stomach, and colon lining
-
Imaging Studies: Ultrasound, CT scan for structural abnormalities
-
Laboratory Tests: H. pylori breath or stool test, stool cultures, inflammatory markers (CRP, calprotectin)
-
Functional Tests:
-
Hydrogen breath test for lactose/fructose intolerance or SIBO
-
Gastric emptying study for gastroparesis
-
-
-
Antacids & Mucosal Protectants:
-
Aluminum/Magnesium hydroxide, Sucralfate for rapid heartburn relief
-
-
H₂-Blockers:
-
Ranitidine, Famotidine to reduce acid secretion
-
-
Proton-Pump Inhibitors (PPIs):
-
Omeprazole, Pantoprazole for ulcer healing and GERD control
-
-
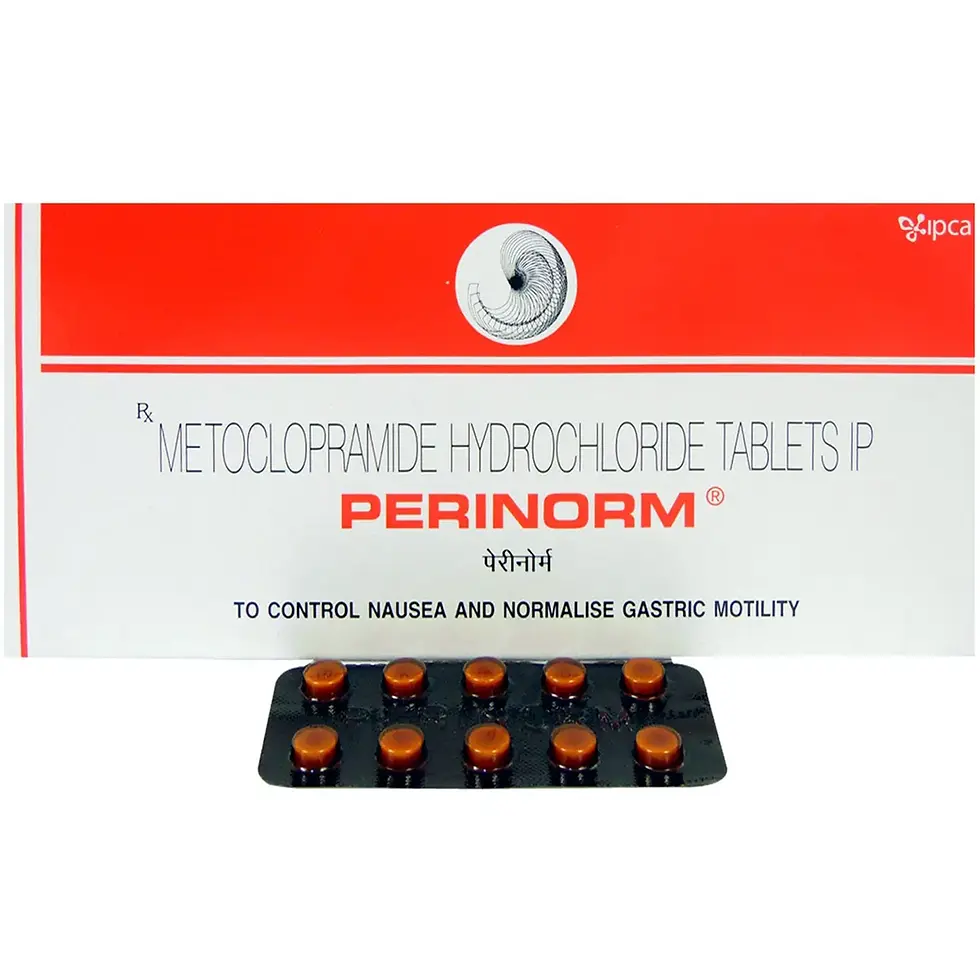
Prokinetics:
-
Domperidone, Metoclopramide to enhance gastric emptying and reduce nausea
-
-
Laxatives & Stool Softeners:
-
Lactulose, Psyllium husk, Docusate for constipation relief
-
-
Antidiarrheals:
-
Loperamide, Racecadotril to firm stools and reduce frequency
-
-
Symptom-Targeted Therapies:
-
Spasmolytics (Dicyclomine) for IBS cramps
-
5-ASA agents for mild inflammatory bowel disease
-
-
Lifestyle & Diet:
-
Eat smaller, frequent meals; increase dietary fiber; avoid trigger foods; manage stress
-
-
Q1: How long should I take a PPI?
A: Standard courses last 4–8 weeks; long-term use requires medical supervision to avoid nutrient malabsorption.
Q2: Can I use antacids daily?
A: Occasional use is fine, but chronic heartburn should be evaluated—overuse can disrupt mineral balance.
Q3: What helps constipation besides laxatives?
A: Adequate hydration, regular exercise, and high-fiber foods (fruits, vegetables, whole grains) promote natural bowel movements.
Q4: When should I be concerned about diarrhea?
A: Seek care if it lasts >2 days, contains blood, or is accompanied by high fever or dehydration.
Q5: Are probiotics beneficial?
A: Many find relief in bloating and stool regularity; choose a multi-strain probiotic and use for at least 4–6 weeks.